
A couple of months ago, the mpox outbreak seemed poised to overwhelm the United States. Cases were, in some instances, doubling every week with no signs of slowing down.
However, the outbreak has taken a dramatic turn in the right direction.
The average number of daily cases has fallen to six, as of Dec. 7, according to the Centers for Disease Control and Prevention. What’s more, the Biden administration announced last week it would let the emergency declaration expire in January.
Public health experts told ABC News that the combination of people changing their behaviors and a strong vaccination campaign helped beat back the disease.
“This really, I think, is a good success story of patients, and really the general public, taking steps to protect themselves,” Dr. Dana Mazo, an infectious diseases specialist and clinical associate professor of medicine at NYU Langone Health, told ABC News. “For patients, hearing what the data is, hearing what the recommendations were and really doing what they could to protect themselves and their communities.”
Vaccine rollout
Currently, the JYNNEOS vaccine, a two-dose vaccine approved by the Food and Drug Administration to prevent smallpox and mpox, is the only vaccine being used in the U.S.
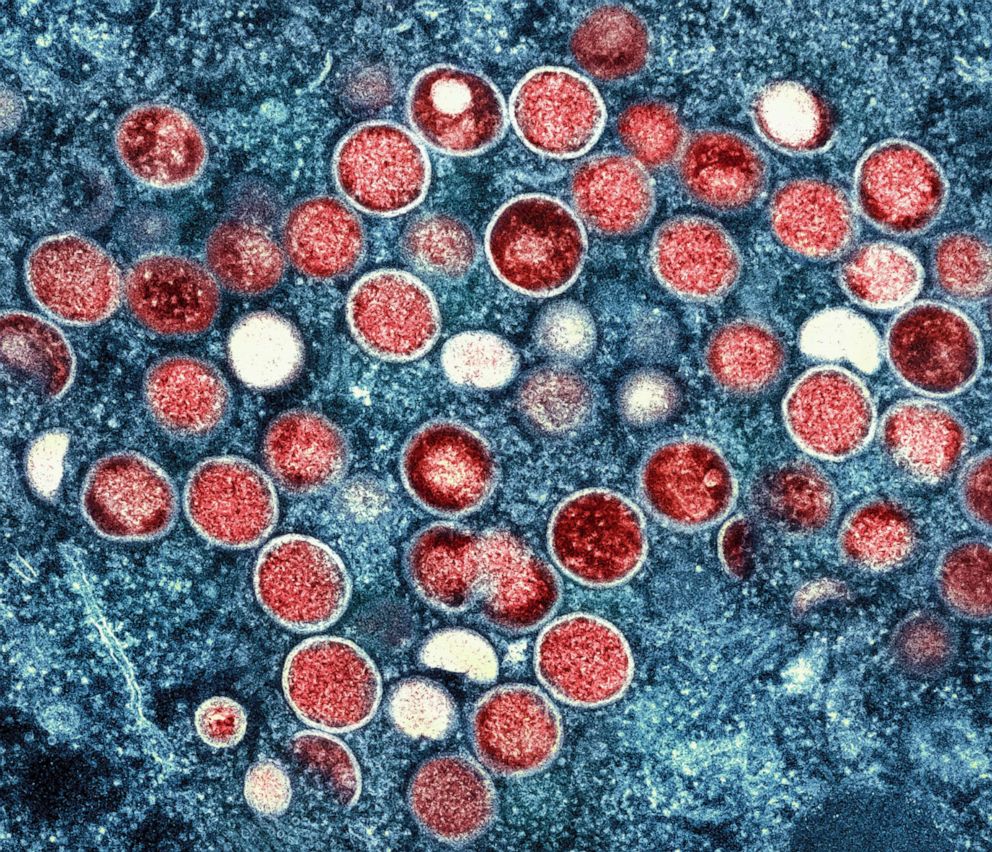
This image provided by the National Institute of Allergy and Infectious Diseases (NIAID) shows a colorized transmission electron micrograph of monkeypox particles (red) found within an infected cell (blue), cultured in the laboratory that was captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Md.
AP, FILE
Data from Africa has shown two doses of JYNNEOS are at least 85% effective in preventing mpox infection.
To increase the number of JYNNEOS doses available, the FDA authorized a proven strategy in August to inject the vaccine intradermally, just below the first layer of skin, rather than subcutaneously, or under all the layers of skin.
This allows one vial of vaccine to be given out as five separate doses rather than a single dose.
Dr. Daniel Kuritzkes, chief of the division of infectious diseases at Brigham and Women’s Hospital, told ABC News that during the early weeks of the outbreak, there were concerns around vaccine supply, so only those with limited or suspected exposures were recommended for vaccination.
“But then as the supply was expanded through the intradermal dosing, it became more feasible, especially in those cities where there were the highest numbers, to broaden vaccination to people potentially at risk, and even without known exposures or suspected exposures,” he said. “And I think that did play an important role.”
As of Dec. 6, more than 1.1 million doses of the vaccine have been administered in the U.S., CDC data shows.
Public changing their behaviors
The experts said another reason for the decline is that Americans who were the most at-risk changed their behaviors.
“The most important [factor] was really effective messaging by public health authorities in close collaboration with affected communities, to help educate people about mpox in a way that wasn’t stigmatizing,” said Kuritzkes.
He continued, “And in order for people to be able to both recognize the signs and symptoms of infection, and then not only get treatment for themselves, but take appropriate measures to prevent transmission to others, but also ways in which people if not yet exposed and not yet infected, could minimize their chances of becoming infected with mpox.”
The outbreak has primarily been concentrated in men who have sex with men, a group that includes people who identify as gay, bisexual, transgender and nonbinary, although health officials have said anyone — regardless of sexual orientation — is at risk if they have direct contact with an infected patient.

Irina Martinez, a registered nurse, administers an intradermal monkeypox vaccine to Britney Castaneda at a vaccination site setup in Tropical Park by Miami-Dade County and Nomi Health, Aug. 15, 2022 in Miami, Florida.
Joe Raedle/Getty Images, FILE
But this group listened to doctors’ advice on how to lower their risk and followed suit, experts said.
A joint survey from the CDC, Emory University and Johns Hopkins University found about one-half of gay, bisexual, and other men who have sex with men reduced their number of sexual partners, one-time anonymous partners, and reduced use of dating apps.
“So really, people responded to the data that was coming out saying that this bulk of the transmission is from casual sexual encounters, and really changed their behavior,” Mazo said.
Not taking foot off the gas
Experts told ABC News even if the number of cases has substantially declined, it doesn’t mean that the threat of mpox has been eliminated.
“I would be cautious about claiming victory, I think it would mean that we were really successful in bringing this epidemic to a close, but we need to remain vigilant,” Kuritzkes said.
They also encourage Americans to get vaccinated against mpox if they are at risk.
Although the disease does not spread through airborne droplets but rather from close, personal, often skin-to-skin interactions, including hugging, touching and prolonged face-to-face contact, the risk is still higher as Americans gather together for the holidays.
Vaccination “is still important, especially because we will see what happens, in the wintertime, when people perhaps are going to be inside more and sort of sharing spaces, again, holiday parties, other things,” Mazo said. “I would still recommend to my patients who are at risk to consider vaccination and discuss vaccination with them, because it would be the best way to protect themselves.”